Vitamin D And Heart Palpitations

- Several studies have linked vitamin D deficiency to coronavirus infection and more severe COVID-19.
- Experts are now investigating if taking vitamin D may help protect against severe COVID-19 symptoms.
- Even before these studies are finished, there are good reasons to consider taking a vitamin D supplement.
All data and statistics are based on publicly available data at the time of publication. Some information may be out of date. Visit our coronavirus hub and follow our live updates page for the most recent information on the COVID-19 pandemic.
With no coronavirus vaccines approved for full use, many people are turning to vitamins and other supplements to bolster their immune system and help them fight off COVID-19.
While plenty of posts on social media push these supplements as personal coronavirus shields, Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases, cautioned last month that most "so-called immune boosting supplements" actually do "nothing."
However, there is one supplement that may be of use to the immune system — vitamin D, also known as the "sunshine vitamin."
"If you are deficient in vitamin D, that does have an impact on your susceptibility to infection," Fauci said in an Instagram Live interview with actress Jennifer Garner. "So I would not mind recommending — and I do it myself — taking vitamin D supplements."
Fauci was not speaking about COVID-19 specifically, but about vitamin D's general role in supporting the immune system — in particular, about the benefits of this nutrient for people who are deficient.
Right now, the National Institutes of Health says there's not enough evidence to show that vitamin D can prevent or treat COVID-19.
But there is enough evidence that scientists are exploring the benefits of this and other supplements against the coronavirus.
Earlier
More recent research suggests that vitamin D deficiency may increase the risk of coronavirus infection and severity of COVID-19.
For example, some studies found that COVID-19 deaths tend to be higher in countries farther away from the equator, where many people are deficient in vitamin D due to the reduced amount of sunlight, especially during winter.
"We make vitamin D by being exposed to sunlight, and in the colder months people can become deficient," said Nicole Avena, PhD, an assistant professor of neuroscience at the Icahn School of Medicine at Mount Sinai in New York.
Many factors could account for the greater number of COVID-19 cases in more northerly latitudes. But a study published last month in
"In our study, patients who have lower vitamin D levels were more likely to test positive for COVID-19," said study author Dr. David Meltzer, a professor of medicine at The University of Chicago Medicine.
This trend still held when they tried to control for other factors — age, obesity, other medical conditions — that might worsen COVID-19 and are linked to lower vitamin D levels.
Other studies show that patients with lower vitamin D levels who are diagnosed with COVID-19 tend to have worse outcomes.
One of these was published last month in
Not all research, though, supports the link between vitamin D and COVID-19.
A UK biobank study published earlier this year in Diabetes & Metabolic Syndrome: Clinical Research & Reviews found no link between vitamin D levels and coronavirus infection.
However, Meltzer and his colleagues pointed out in their paper that the UK researchers measured vitamin D levels up to 14 years before COVID-19 testing and didn't look at whether people had been treated with vitamin D since then.
This could have weakened the observed link between vitamin D levels and coronavirus infection, they wrote.
Scientists are also eyeing other nutrients as potential treatments for COVID-19, including zinc and vitamin C, both touted for their cold-fighting benefits.
In one study, researchers from Spain reported that patients with low blood levels of zinc were more likely to die from COVID-19.
Their results were presented last week at the European Society of Clinical Microbiology and Infectious Disease (ESCMID) Conference on Coronavirus Disease. This research has not been peer-reviewed, so it should be viewed with some caution.
All of these studies are observational, meaning researchers collected data on people over time, rather than assigning people to different treatments. That makes it impossible to show a cause-and-effect relationship between vitamin D and COVID-19.
What's needed are randomized controlled trials (RCTs), the "gold standard" of clinical research. Some of these are already underway.
In one study carried out in Spain, researchers gave calcifediol, an active form of vitamin D, to 50 people hospitalized with COVID-19. Another group of 26 patients didn't receive vitamin D.
All patients were treated equally with hydroxychloroquine and azithromycin.
Only one of the patients treated with vitamin D ended up in the intensive care unit, while half of the untreated patients did.
"There are some imperfections [to the study] — it's not a very large study, there are some slight imbalances between the groups — but it's pretty impressive," said Meltzer.
While this study used vitamin D to treat people who already had COVID-19, Meltzer says the nutrient might work equally well at keeping people out of the hospital.
"One possibility is that vitamin D is not preventing COVID-19," he said, "but is causing people who are infected to have such minimal symptoms that they never get tested, never get found."
More research is needed to know if this is true.
Two randomized controlled trials starting at the University of Chicago should provide some answers. In both, people will be treated with vitamin D and then followed to see if they contract the coronavirus and how severe their symptoms are.
One trial focuses on healthcare workers. The other will recruit people from the community, with an emphasis on enrolling Black and Hispanic people, who are at high risk for both vitamin D deficiency and COVID-19.
At the Cleveland Clinic, researchers are enrolling people into a study to see if vitamin C or zinc — or a combination of the two — can reduce the duration of COVID-19 symptoms. Patients will be given the supplements after they have tested positive for COVID-19.
How soon results are available from these studies depends on how quickly researchers can enroll people into the studies. Meltzer says study volunteers are essential for the success of COVID-19 research.
"People who can enter clinical trials do a tremendous service to society," he said.
Although Meltzer is enthusiastic about the potential benefits of vitamin D, he cautions that we won't really know until the randomized controlled trials are finished.
"This doesn't mean we should let down our guard or not do any of the other things we're doing," he said. "I certainly wouldn't stop wearing a mask and go to a big party thinking everything was going to be OK because I was taking vitamin D."
Even before these studies are finished, there are good reasons to consider taking a vitamin D supplement.
"The vast majority of Americans are vitamin D deficient and could probably benefit from some modest level of vitamin D supplementation, at very little risk," said Meltzer.
In the United States, an estimated
Other factors increase the risk of vitamin D deficiency, including age, limited sun exposure, obesity, and certain medical conditions.
Avena says it is difficult to get enough vitamin D from foods. "So taking a supplement may be advised," she says, "but always check with your doctor first."
Meltzer says he takes 4,000 international units (IU) per day. The National Institutes of Health says this is the upper limit of what is
"Don't consume more than 4,000 IU per day of vitamin D without your doctor's permission," said Avena. "It exceeds the safe upper limits of intake."
Larger doses can be toxic and should only be taken under medical supervision.
Avena says zinc may also be helpful once you feel symptoms of a
She recommends taking between 13.3 milligrams and 23 milligrams of zinc every 2 hours while you have cold symptoms, but no longer than 1 week. This is the dose found in over-the-counter gummies and lozenges.
As with vitamin D, we don't yet know if zinc will reduce symptoms of COVID-19.
While most people get enough zinc from food sources,
Vitamin D And Heart Palpitations
Source: https://www.healthline.com/health-news/what-to-know-about-vitamin-d-and-covid-19








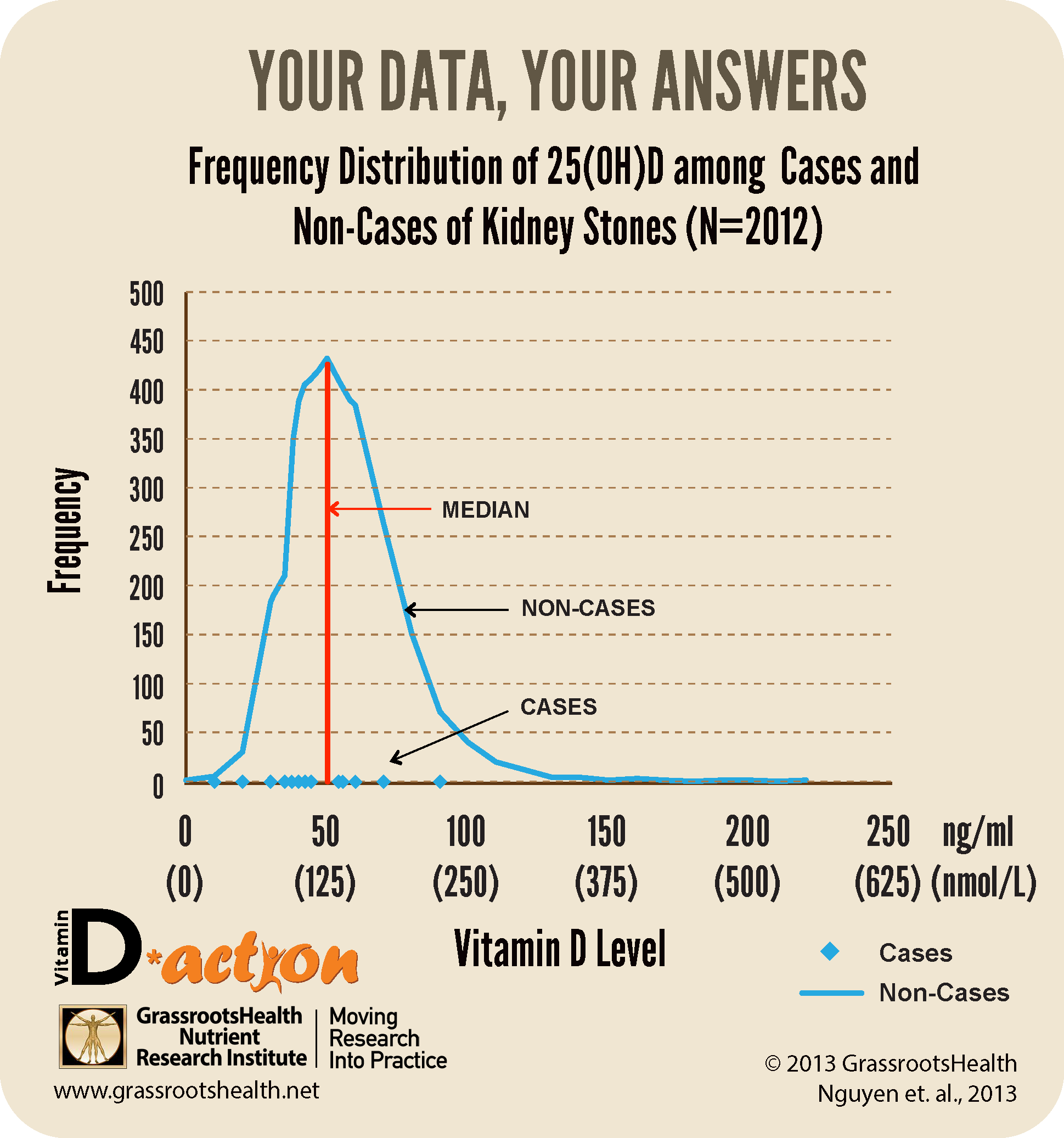
 Kidney stones are hard, crystallized deposits made of salts and minerals, such as calcium and phosphate, which form inside the kidneys. Often these stones must be passed out in the urine and can become stuck in the urinary tract which results in incredible pain. There are many known causes for these deposits, including drinking too little water and eating foods high in purines – a chemical compound that occurs naturally in your body but is also found in foods and drinks, such as beer and other yeasty beverages.
Kidney stones are hard, crystallized deposits made of salts and minerals, such as calcium and phosphate, which form inside the kidneys. Often these stones must be passed out in the urine and can become stuck in the urinary tract which results in incredible pain. There are many known causes for these deposits, including drinking too little water and eating foods high in purines – a chemical compound that occurs naturally in your body but is also found in foods and drinks, such as beer and other yeasty beverages.